Making the complex more convenient
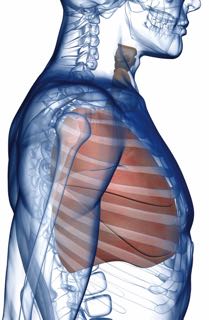 The surgery team that treats the lungs, esophagus and chest is safely extending the possible benefits of minimally invasive surgery, including reduction of pain and a decrease in the length of hospital stay, to one of the most complex areas of medicine.
The surgery team that treats the lungs, esophagus and chest is safely extending the possible benefits of minimally invasive surgery, including reduction of pain and a decrease in the length of hospital stay, to one of the most complex areas of medicine.
Keith Mortman, MD, FACS, FCCP, Director of Thoracic Surgery, and Gregory Trachiotis, MD, FACS, FCCP, Chief of Cardiothoracic and Thoracic Surgery, make up the thoracic surgical team that performs a range of procedures, from lobectomy – where the cancerous portion of a lung is removed – to a sympathectomy, to cure profuse sweating.
Technology supporting the team at the George Washington University Hospital includes a da Vinci® robot, and a minimally invasive surgical approach is seen as a benefit to both the patient and the surgeon.
It’s not just about the incision
While the incisions used when performing minimally invasive thoracic surgery are smaller than those of a traditional, open operation, this isn’t the primary reason for a reduction in pain. It’s because the surgeon doesn’t have to spread the patient’s ribs apart to view the operative area. “Many procedures can be performed through the single-port video technique, an advancement made because of better cameras and tools to perform thoracic procedures,” says Dr. Trachiotis.
With today’s high-definition endoscopes – which comprise tiny but powerful cameras – surgeons can see more detail, and the tools used to navigate tight spaces during the operation are exceptionally slim. “Also, in partnering with our cardiothoracic anesthesiologists, special modalities such as thoracic epidural catheters can lead to improved pain control, pulmonary function and recovery in the hospital,” he adds.
“Often, we can see better than if we were looking through an open incision, because you can only spread the ribs apart so far,” says Dr. Mortman. “The endoscope brings light inside, and lets you see throughout the chest. You can get way up into the apex or way down, and if you have to go further, you advance the endoscope, which doesn’t increase pain.”
Confidence comes from a skilled medical team
Part of an academic medical center and teaching hospital for residents, the George Washington University Hospital thoracic surgery department includes physicians who have published their work in medical journals
and who lecture nationally and internationally.
Support staff complements these credentials, and includes a physician’s assistant, Kevin Dubree, PA-C, who has 17 years’ experience, and a nurse navigator, Meg Flood,
RN. The latter helps smooth the surgical experience by talking with patients, setting up appointments, ensuring studies are up to date, ordering pre-operative testing, handling paperwork and assisting with post-op follow-up.
Since about half of the patients seen have had a cancer diagnosis, the team communicates closely with specialists like pulmonologists, radiation oncologists and medical oncologists in a weekly thoracic oncology conference to discuss test results, complications and plan the next steps for patients. In this way, each aspect of a patient’s case is considered from a wide perspective, and treatment is tailored individually.
“When you choose GW Hospital, you’re choosing a medical staff of physicians who are leaders in their fields, with outcomes that meet or exceed national benchmarks,” says Dr. Mortman. “The specialists here want to obtain the best outcome for each patient.”
Read more about thoracic surgery at GW Hospital

