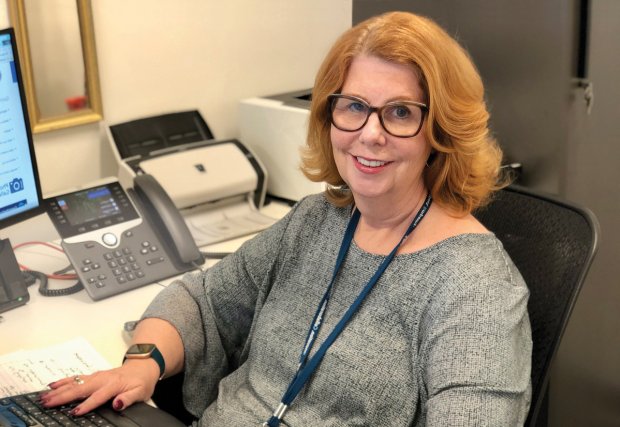
Arlene Bright is an accomplished nurse and mother who struggled for years with a problem that many women face, but few talk about: urinary incontinence. It began with occasional leaks and gradually worsened to the point where she’d lost all bladder control. Not only was it upsetting, it was painful and embarrassing. “I had to hope this didn’t happen in the middle of meetings and events I was committed to,” she says.
For years, she thought her symptoms were caused by an overactive bladder, but testing later showed that she also had pelvic organ prolapse and stress urinary incontinence. Prolapse occurs when the muscles and ligaments supporting the pelvic organs weaken or tear due to childbirth, aging or other factors, causing one or more of the pelvic organs to drop from their normal position. Stress incontinence is leaking with coughing, laughing, sneezing and sometimes running or lifting.
 Urogynecology specialist Charelle Carter-Brooks, MD, MSc, who provides care at the GW Pelvic Floor Center, explains that pelvic floor disorders like Arlene was experiencing are actually quite common, affecting anywhere from one-quarter to one-third of women in their lifetime. “Many women do not seek care because they are embarrassed, unaware of treatment options or have accepted their condition as part of aging,” she says.
Urogynecology specialist Charelle Carter-Brooks, MD, MSc, who provides care at the GW Pelvic Floor Center, explains that pelvic floor disorders like Arlene was experiencing are actually quite common, affecting anywhere from one-quarter to one-third of women in their lifetime. “Many women do not seek care because they are embarrassed, unaware of treatment options or have accepted their condition as part of aging,” she says.
Arlene says that when she met with Dr. Carter-Brooks about her condition, she felt heard and validated, and also hopeful that there was a solution. After considering her treatment options, she decided to move forward with a vaginal prolapse repair and a midurethral sling to address the structural issues disrupting her life. The outpatient procedure was done vaginally, with no abdominal incisions, and involved lifting the bladder, vagina and rectum to the normal position and implanting a sling under the urethra to help prevent urinary leakage. The recovery took about three weeks, but Arlene remembers feeling the effects immediately, as her normal functioning returned. “It was truly life-changing,” she says.
Since her recovery, simple things, like being able to get her hair done without making multiple trips to the bathroom, are a joy. Her message to others who may face similar struggles? “There are options ... I did not realize how urogynecology really can change a woman’s life until I went through it myself.”
Know The Signs
If you are experiencing a constant urge to urinate, urinary leakage or feel a bulge coming from your vagina, these are signs to seek care with a urogynecologist. Care is also provided for bowel incontinence, vaginal dryness and other pelvic floor issues. Treatment may range from non-surgical options, like physical therapy, medication or a pessary, to different minimally invasive surgical procedures.
Individual results may vary. There are risks associated with any surgical procedure. Talk with your doctor about these risks to find out if minimally invasive surgery is right for you.