It is important for every woman to know her breast density because it impacts her breast cancer risk, as well as how well mammograms can detect breast cancer. The only way to know your breast density is by the results of your mammogram.
What’s in the Number?
Doctors use The American College of Radiology’s Breast Imaging Reporting and Data System (BI-RADS) scoring method using a 1-4 rating system. This classification system allows radiologists to measure and describe breast density
- BI-RADS 1- less than 25% Dense Breast Tissue
- BI-RADS 2 - 26-50% Dense Breast Tissue
- BI-RADS 3 - 51- 75% Dense Breast Tissue
- BI-RADS 4 - more than 75% Dense Breast Tissue
Podcast: What You Need to Know About Breast Health
Rachel F. Brem, MD, FACR, FSBI, discusses the various breast cancer screening options (mammography, ultrasound, MR, molecular breast imaging) and clears up some of the confusion surrounding the current mammography recommendations. Dr. Brem also explains the advances in biopsy procedures, as well as why early detection is crucial in preserving women's lives.
At the GW Breast Center, radiologists who interpret your mammograms will let you know your breast density along with the results of your mammogram because it impacts your risk of breast cancer. Several states in the nation, including Virginia, now require women be told their breast density, but currently Maryland and DC do not.
What is breast density? And how does it impact my risk for cancer?
Breast Density is a measure of the amount of breast tissue a woman has. The more tissue, the greater the density and the higher the risk of breast cancer. However, in women with dense breast tissue, mammograms are not as effective in detecting the cancer. This is because both breast tissue and breast cancer will appear white on a mammogram and the lack of contrast makes identification of the cancer more difficult.
Digital mammography is the standard to detect early curable breast cancer. Mammography is effective and is probably the most important reason that smaller more curable breast cancers are being detected and that the death rate from breast cancer is decreasing. However, the ability of mammography to detect breast cancer in women with dense breast tissue is limited.
The issue of breast density is important. Nearly half of all women in the United States have dense breast tissue. Women with dense breasts are at a 4-6 times higher risk of developing breast cancer than women who do not.
Although breast density is loosely associated with age, with nearly three-fourths of women in their 30s having dense breast tissue, more than a quarter of women in their 70s also have dense breast tissue.
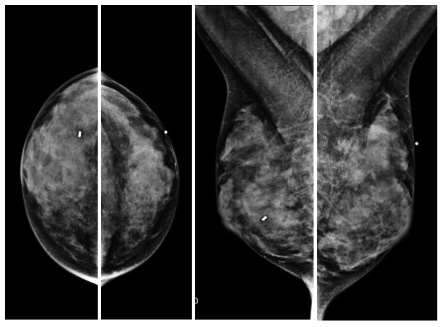
Below is an example of a mammogram from a woman with dense breast tissue and a large breast cancer. The dense tissue appears white, just as the tumor does, causing the breast tissue to mask the cancer. This is why more than one third of breast cancers are missed by mammography in women with dense breasts.
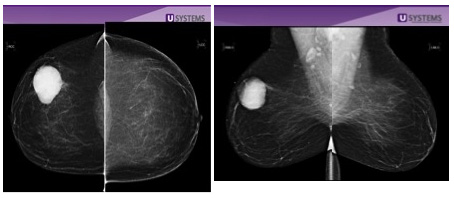
By comparison, below is an example of a breast cancer in a woman with non-dense breast tissue. The white tumor (circle) in the right breast is easily visible against the dark gray and black non-dense tissue.
Dense Breasts and Other Breast Cancer Risk Factors
Breast cancer is one of the most frequently diagnosed cancers among women. The majority of women diagnosed with breast cancer have no known family history or other risk factors. Only 5-10 percent of breast cancers are due to a genetic cause. That’s why screening for breast cancer is so important. The most significant risk factors for breast cancer includes being female and age. However, increased breast density is a strong independent risk factor for developing breast cancer. The reason it is so important for women to be aware of their breast density is that there are other approaches, in addition to mammography, which can help detect breast cancers which would not be seen with mammography alone such as Automated Breast Ultrasound (ABUS), Breast Specific Gamma Imaging (BSGI) and Magnetic Resonance Imaging (MRI).